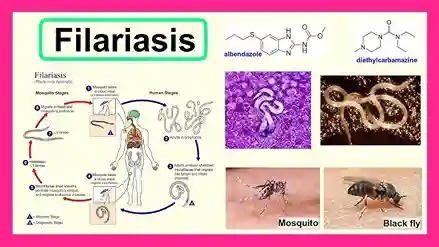
Filariasis
Filariasis is a group of infections caused by filarial worms that can affect both animals and humans. There are many types of filarial parasites, there are hundreds of types, but only eight species can cause infection in humans.
Filariasis grouping is generally categorized according to the location of the adult worm habitat in the human body, namely skin, lymphatic, and body cavity filariasis. Lymphatic filariasis is the most common condition or better known as elephantiasis .
Symptoms of Filariasis
Based on symptoms, lymphatic filariasis is divided into three categories which include asymptomatic, acute, and chronic conditions.
-
Asymptomatic
Most lymphatic filariasis infections are asymptomatic, but they can cause damage to the lymph nodes and kidneys and affect the immune system.
-
Acute lymphatic filariasis
This condition is divided into two types, namely:
- Acute adenolymphangitis (ADL)
Symptoms that appear are fever, swelling of the lymph or lymph nodes (lymphadenopathy), and the infected body part will feel sore, red, and swollen. ADL can recur more than once a year. Accumulated fluid can trigger fungal infections of the skin that damage the skin. The more frequent the recurrence, the more severe the swelling can be.
- Acute filarial lymphangitis (AFL)
AFL is caused by dying adult worms that will trigger slightly different symptoms than ADL because it is usually not accompanied by fever or other infections. In addition, AFL can trigger symptoms that include the appearance of small lumps on the body, where the dying worms collect (for example in the lymph system or in the scrotum).
-
Chronic lymphatic filariasis
This condition will cause lymphedema or fluid buildup that causes swelling in the legs and arms. The accumulation of fluid and infections that occur due to weak immunity will eventually lead to damage and thickness of the skin layer. This condition is called elephantiasis. In addition, fluid buildup can also affect the abdominal cavity, testicles in men and breasts in women.
Causes of Filariasis
According to WHO, there are around 120 million people in the world who suffer from lymphatic filariasis and one third of them have severe infections. The filarial parasite enters the human body through the bite of an infected mosquito. The worms will grow into adults, survive for six to eight years, and continue to reproduce in the human lymph tissue.
This infection is usually experienced since childhood and causes damage to the lymphatic system that is not noticed until it eventually causes severe and painful swelling. The swelling can then cause permanent disability.
Risk Factors for Filariasis
There are several risk factors for filariasis, namely:
- Prolonged exposure to mosquitoes and repeated bites.
- People who live long periods in tropical or subtropical areas.
- People who are accustomed to hunting or fishing have an increased risk of filarial antigenemia.
- Warm temperatures and sweating increase the risk of mosquito bites.
Diagnosis Filariasis
The standard method for diagnosing active filariasis infection is through microscopic identification of microfilariae in a blood smear. The microfilariae that cause lymphatic filariasis circulate in the blood at night (called nocturnal periodicity).
Blood should be drawn in the evening when microfilariae appear, and thick smears should be made and stained with Giemsa or hematoxylin and eosin. To increase sensitivity, concentration techniques may be used.
Serological techniques provide an alternative to the microscopic detection of microfilariae for the diagnosis of lymphatic filariasis. Patients with active filarial infection usually have elevated levels of antifilarial IgG4 in the blood and this can be detected using routine tests. Lymphedema may develop many years after infection, and laboratory tests are likely to be negative in these patients.
Filariasis Treatment
Treatment for filariasis varies depending on what symptoms you have and how severe the condition is. In general, filariasis treatment can include:
-
Medicine
You can take anti-parasitic drugs such as ivermectin, diethylcarbamazine, or albendazole. These drugs destroy adult worms in the blood or prevent them from multiplying. Taking these drugs can also prevent the infection from spreading to others. Because the worms may still be alive in your body, you must take these drugs once a year for several weeks.
-
Surgery
You may need surgery to remove the dead worms from your bloodstream. This happens if filariasis has caused a hydrocele, so the only way is to have surgery to remove the buildup of fluid in the scrotum.
-
Management of elephantiasis
Medical staff may also recommend strategies to manage swelling, such as elevation or compression garments.
Recommended Filariasis Medication
There are several drug options that you can use to treat filariasis. Before taking this drug, it is a good idea to consult a doctor first to get a more appropriate dosage or advice.
Here are some recommendations:
- Albendazole 400 mg Chewable Tablets . Albendazole is a worm medicine that works by damaging intestinal cells in worms so that the worms do not absorb sugar and run out of energy and die. This medicine is used to treat single or mixed infections caused by worms.
- Konvermex 125 mg 4 Caplets . Konvermex 125 tablets are a family worm medicine in the form of suspension and tablets with the active ingredient pyrantel pamoate, which can paralyze worms in the body.
- Konvermex 250 mg 2 Caplets t. This medicine is used to treat infections caused by worms. You can use this medicine for your family because it can be used for adults and children.
Complications of Filariasis
Over time, damage to the lymphatic system can make it harder for the body to fight off infections. A decreased immune response can also lead to the development of conditions such as:
- Frequent bacterial infections.
- Elephantiasis, thickened and hardened skin and fluid retention that causes painful, swollen, and enlarged body parts.
- Tropical pulmonary eosinophilia syndrome, an increase in white blood cells that causes coughing and difficulty breathing.
Prevention of Filariasis
The main step in preventing filariasis is to avoid mosquito bites as much as possible. This is very important, especially in tropical countries such as Indonesia. To maximize protection against mosquito bites, we can take simple steps that include:
- Wearing a shirt or trousers.
- Apply mosquito repellent lotion.
- Sleep under a mosquito net.
- Cleaning up puddles of water around the environment.
When to See a Doctor?
Contact a doctor immediately if you experience these symptoms. Proper handling can minimize the effects, so that treatment can be done more quickly.