Pulmonary Edema
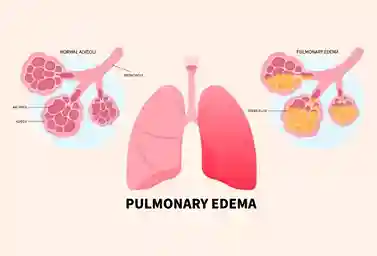
Pulmonary edema is a serious medical condition that occurs when excess or buildup of fluid begins to fill the air sacs in the lungs (alveoli).
When filled with fluid, the alveoli cannot adequately add oxygen, or remove carbon dioxide from the blood.
That is why this condition can cause significant breathing difficulties, and potentially be a life-threatening problem.
Symptoms of Pulmonary Edema
Acute conditions can cause significant breathing difficulties and can appear without warning.
This is an emergency and requires immediate medical attention.
This condition can be fatal without proper treatment and support.
Along with difficulty breathing, other signs and symptoms of acute pulmonary edema may include:
- Cough, often accompanied by the production of bloody sputum.
- Excessive sweating.
- Anxiety and restlessness.
- Feeling of suffocation.
- Pale skin.
- Wheezing.
- Fast or irregular heart rhythm (palpitations).
- Chest pain.
If it is chronic, the symptoms are usually not so severe that the body’s system can no longer compensate. Typical symptoms include:
- Difficulty breathing when lying flat (orthopnea).
- Swelling (edema) of the feet or legs.
- Rapid weight gain due to accumulation of excess fluid.
- Paroxysmal nocturnal dyspnea (sudden episodes of severe shortness of breath at night).
- Fatigue.
- Increased shortness of breath during physical activity.
Causes of Pulmonary Edema
The cause of pulmonary edema depends on its type. Based on the cause, this condition is divided into two, namely cardiogenic and non-cardiogenic.
Here is the review:
-
Cardiogenic
Cardiogenic pulmonary edema occurs when an underlying heart problem causes pressure in the left side of the heart to become high.
This high pressure is transmitted backward, through the pulmonary veins, to the alveolar capillaries.
Due to increased pulmonary capillary pressure, fluid leaks out of the capillaries into the alveolar air spaces, and edema occurs.
Almost any type of heart disease can eventually lead to increased pressure on the left side of the heart and trigger edema.
The most common types of heart disease that cause pulmonary edema are:
- Coronary artery disease.
- Heart failure, such as congestive heart failure.
- Heart valve disease, especially mitral stenosis, mitral regurgitation, aortic stenosis, or aortic regurgitation.
- Severe hypertension.
-
Non-Cardiogenic
The alveoli can also fill with fluid for reasons unrelated to increased cardiac pressure.
This can occur when capillaries in the lungs become damaged and “leaky”, allowing fluid to enter the alveoli.
The most common cause of non-cardiogenic pulmonary edema is acute respiratory distress syndrome (ARDS), which is caused by diffuse inflammation within the lungs.
Inflammation damages the walls of the alveoli and allows fluid to accumulate.
ARDS usually occurs in critically ill patients and can result from infection, shock, trauma, and several other conditions.
Apart from ARDS, non-cardiogenic pulmonary edema can also occur due to:
- Pulmonary embolism can cause a number of symptoms. If you want to know more about it.
- Located at an altitude of over 2,400 meters above sea level.
- Drug use (especially heroin and cocaine).
- Viral infection.
- Poisons (e.g., inhalation of chlorine or ammonia).
- Neurological problems (such as brain trauma or subarachnoid hemorrhage).
- Inhaling smoke, especially from fires, contains chemicals that can damage the membranes between the air sacs and capillaries.
- Almost drowned.
Pulmonary Edema Risk Factors
There are many factors that can increase the risk of pulmonary edema in a person, namely:
- Viral infection.
- Acute respiratory distress syndrome or acute respiratory distress syndrome.
- Pulmonary embolism.
- Injury to the lungs.
- Having an accident such as drowning.
- The center is at an altitude (up to more than 2,400 meters above sea level).
- Being overweight or obese.
- Having a head injury, seizure, or after brain surgery.
- Inhaling smoke during a fire. Exposure to ammonia and chlorine toxins, which may occur during a train accident.
- Addiction to stimulant drugs.
Pulmonary Edema Diagnosis
You can diagnose pulmonary edema through a medical interview, physical examination, and supporting examinations.
You should immediately install pulse oximetry to quickly measure the oxygen levels in the patient’s blood.
Meanwhile, supporting examinations that you also need for the examination:
- Electrocardiography (ECG), to check for signs of heart attack and problems with heart rhythm.
- Chest X-ray, to ensure that the sufferer is really experiencing it, and to look for other possible causes of shortness of breath.
- Blood tests, to measure the levels of oxygen and carbon dioxide in the blood, measure levels of the hormone B-type natriuretic peptide (BNP) which is elevated in heart failure, and look at thyroid and kidney function.
- Echocardiography, to detect problems with the heart muscle.
- Cardiac catheterization, which you can do if the condition appears with chest pain, but the doctor cannot find any abnormalities on the ECG or echocardiography.
- Pulmonary artery catheterization, to measure the pressure within the blood vessels of the lungs.
Pulmonary Edema Treatment
Pulmonary edema is a serious condition that requires immediate treatment. Treatment for pulmonary edema may include:
-
Oxygen administration
Oxygen may be the first-line treatment for this condition, depending on its severity.
Through oxygen administration, doctors can support the sufferer and provide 100 percent oxygen. Through an oxygen mask, nasal cannula, or positive pressure mask.
-
Administration of diuretic drugs
In less severe cases, pulmonary edema can also be treated with diuretics or water pills.
When receiving this treatment, people with pulmonary edema may not have to stay in the hospital.
-
Treatment of the underlying condition
A doctor will also diagnose the cause of pulmonary edema and prescribe appropriate treatment for the underlying cause.
Depending on the condition and cause, your doctor may also prescribe:
- Preload reducers. These drugs help reduce the pressure of fluid entering the heart and lungs. In addition, the use of diuretic drugs can also help reduce this pressure. This is because diuretic drugs make people with this condition urinate frequently, so they can eliminate fluid.
- Reducing afterload. These drugs widen blood vessels and take pressure off the heart.
- Heart medication. This medication will control your heart rate, reduce high blood pressure, and reduce pressure on your arteries and veins.
- Morphine. This drug is commonly used to relieve anxiety and shortness of breath. But fewer doctors today use morphine because of the risks.
- Intensive or critical care. In severe cases, people with pulmonary edema may need intensive or critical care.
In other cases of pulmonary edema, the sufferer may need treatment to help him or her breathe.
A machine will deliver oxygen under pressure to help get more air into the lungs.
Sometimes this procedure can also be performed by the doctor using a mask or cannula or continuous positive airway pressure (CPAP).
In addition to these treatment methods, there are several other efforts that pulmonary edema sufferers can make to help the healing process, namely:
- Do not smoke.
- Lose weight if you are overweight.
- Reduce consumption of alcoholic beverages.
- Exercise regularly.
- Reduce salt intake in food.
Pulmonary Edema Medication Recommendations
There are several medications that can be used to help the healing process and treat the symptoms of pulmonary edema. Here are the options:
- Nitrocaf Retard 2.5 mg 10 Capsules . This medicine contains nitroglycerin with long-term effects for patients with pulmonary edema (if caused by heart problems) or angina pectoris.
- Nitrokaf Retard Forte 5 mg 10 Capsules. Contains nitroglycerin which is a drug for long-term therapy, for pulmonary edema (if caused by heart disorders) ,or angina pectoris sufferers.
- Furosemide 40 mg 10 Tablets t. Furosemide is one of the drugs that can be used to treat fluid buildup in the body.
- Amlodipine 10 mg 10 Tablets . Amlodipine is an antihypertensive drug used to treat one of the symptoms of pulmonary edema, namely irregular heart rhythm.
Foods and Drinks to Avoid for Pulmonary Edema Sufferers
There are a number of foods and drinks that people with pulmonary edema need to avoid, including:
- High-sodium foods. Certain types of salty foods that are high in sodium make the body work harder to retain water to dilute and process it. This condition can trigger edema or make it worse if you already have it.
- High-fat foods. It is important to avoid consuming high-fat foods such as fried foods. Because excessive fat intake can cause obesity. When obesity occurs, mechanical compression can occur on the diaphragm, lungs, and chest cavity. This condition can cause restrictive lung damage.
- Limit your consumption of sweet foods. If you have diabetes, be sure to limit your sugar intake. This is because pulmonary edema can occur due to uncontrolled diabetes.
- Alcoholic Beverages. Chronic (prolonged) alcohol abuse poses a higher risk of threatening the life of people with pulmonary edema.
Complications of Pulmonary Edema
Complications depend on the cause. However, in general, if the condition persists, the pressure in the pulmonary artery can increase (pulmonary hypertension).
Eventually, the heart becomes weak and begins to fail, and the pressure on the heart and lungs increases.
In addition, here are some complications of pulmonary edema that can also occur:
- Difficulty breathing.
- Swelling of the legs, feet and abdominal area.
- Accumulation of fluid in the membrane surrounding the lungs (pleural effusion).
- Liver congestion and swelling.
- Immediate treatment is needed for acute pulmonary edema to prevent death.
Prevention of Pulmonary Edema
If you are at high risk of developing it, it is important to follow your doctor’s advice to keep the condition under control.
If congestive heart failure is the problem, healthy lifestyle changes and maintaining a healthy weight can help reduce the risk.
In general, some prevention tips that you can do are:
- Regular exercise.
- Reduce salt intake.
- Lowers cholesterol levels.
- Quit smoking.
You can minimize high-altitude pulmonary edema by climbing gradually, taking medication before traveling, and avoiding excessive activity when climbing to higher altitudes.
When to See a Doctor?
Immediately check your condition with a doctor if you experience:
- Shortness of breath, especially if it occurs suddenly.
- Difficulty breathing or feeling of suffocation.
- A gasping sound when breathing.
- Phlegm is pink and frothy when coughing.
- Difficulty breathing with excessive sweating.
- A bluish or grayish color to the skin.
- A significant drop in blood pressure that causes dizziness, weakness or sweating.
- Sudden worsening of symptoms associated with chronic pulmonary edema or altitude.
Contact a doctor immediately if you experience these symptoms.
Fast and appropriate handling can minimize the consequences so that treatment can be carried out more quickly.